— Dawn M. Sweet, Ph.D.
Low calorie diets, lifestyle changes, and meal replacements are more reliable for long-term weight loss.
Ozempic and Wegovy have garnered much attention because of their efficacy in helping adults with obesity lose weight. Wegovy was developed as a weight loss drug while Ozempic, a drug developed as a diabetes medication, is now noted for its off label use for weight loss. Although Ozempic and Wegovy have been found to help persons with obesity lose weight, they are not a necessarily foolproof approach for long-term weight loss and weight management.
As with any drug, Ozempic and Wegovy have drawbacks. Commonly reported side effects include hair loss, nausea, diarrhea and vomiting.1,2 Additionally, Ozempic and Wegovy are cost prohibitive for many patients who must pay out of pocket. According to reports from PBS and Bloomberg, patients can pay as much as $1,000 per month3 — an expense that would extend across the rest of their lives.4 Perhaps the side effect that may be of most interest to adults with obesity is weight gain. Research has found that two-thirds of the weight people lost was regained once they stopped taking Ozempic or Wegovy.5 This finding is in stark contrast to research that shows lifestyle changes and meal replacements as part of low calorie diet (LCD) are a proven strategy for weight loss and weight maintenance.
Semaglutide, Side Effects and Weight Regain
The active ingredient in Ozempic and Wegovy is Semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1RA). GLP-1RAs have demonstrated efficacy in improving glycemic control and facilitating weight loss.6 A 2021 study on the side effects of Semaglutide includes GI issues as well as increases in one’s risk of cholelithiasis.6 GLP-1RAs have also been linked to pancreatitis.
In a 20225 study investigating weight regain, 232 patients who were administered Semaglutide were compared to 101 patients who received a placebo. While Semaglutide demonstrated greater efficacy for weight loss, resulting in a 17.3 percent mean weight loss compared to 2.0 percent mean loss for the placebo group, once Semaglutide was no longer administered, those in the Semaglutide group regained 11.6 percent of body their weight, compared to only 1.9 percent in the placebo group. Patients in the Semaglutide group regained two-thirds of the weight they lost in the year following the withdrawal of Semaglutide. It should be noted that 48.2 percent of Semaglutide patients still maintained clinically relevant weight loss. While maintaining clinically meaningful weight loss is important, it does suggest that Semaglutide alone may not be sufficient for maintaining significant long-term weight loss.
Semaglutide and Low Calorie Diets
While Semaglutide has been shown to help patients with obesity lose weight, it is not a standalone success. Research suggests that when coupled with a low calorie diet (LCD) that includes meal replacements and behavioral therapy, weight loss results were optimized. In a study involving 611 participants (n = 407 in Semaglutide + LCD and behavioral therapy and n = 204 in the placebo group) with a BMI ³ 30.0 kg/m2 or ³27.0 kg/m2 with a comorbidity such as hypertension, high cholesterol, obstructive sleep apnea, or cardiovascular disease, researchers investigated the effects of Semaglutide, a low calorie diet, and behavioral therapy on weight loss. It should be noted that 567 participants completed the trial, with 16.7 percent and 18.6 percent dropping from the treatment and placebo groups respectively. Attrition was attributed to intolerance for Semaglutide and the placebo.
Participants were randomly assigned to the Semaglutide group and the placebo group. During the first eight weeks of the study, participants in both groups followed a low calorie diet (1,000 – 1,500 kcal/d) that included meal replacements such as liquid shakes, meal bars, and portion-controlled meals. Following the eight week low calorie diet, participants transitioned to a hypocaloric diet (1,200 – 1,800 kcal/d) where they consumed conventional food for the balance of the study. Caloric intake was determined by body weight. Participants in the low calorie group were also instructed to get 100 minutes of physical activity each week across four to five days. By week four, participants had to increase their physical activity to 200 minutes. The behavioral intervention was 30 visits with a dietician.
Semaglutide and Lifestyle/Behavioral Changes
Semaglutide coupled with a low calorie diet and behavioral therapy increased weight loss by 10.3 percent compared to the placebo group. Despite the success of the treatment, the authors note that they could not isolate each of the three interventions’ role in the weight loss. Because the authors could not partition out the effect of Semaglutide on weight loss, results do not definitively show that Semaglutide alone is responsible for the increase in weight loss.
The benefits of a low calorie diet when coupled with lifestyle changes such as increased physical activity are well documented.7 Losing weight and maintaining a healthy weight is a significant health challenge for many, with 41.9 percent of adults worldwide currently having obesity and 51 percent of adults worldwide predicted to be living with obesity by 2030.8,9, so when the efficacy of new drugs are being touted, it is easy to get swept up in the frenzy. It is important to note that drugs like Ozempic and Wegovy, whose active ingredient is Semaglutide, are not a panacea and do not represent the Holy Grail of weight loss and weight management.
Semaglutide and Meal Replacements
The tried-and-true traditional approach to weight loss, calorie restriction and exercise are a formidable strategy. Medical grade meal replacements (e.g., pudding shakes or drinks) or discrete foods (e.g., protein bars) offer patients with obesity nutritional benefits, providing them with high quality protein as well as the vitamins and minerals needed as part of a healthy diet.10 Adding 60 grams of lean protein to your diet can help preserve muscle mass and much needed amino acids to promote healthy growth and development. Dietary changes and adding physical activity will better serve patients with obesity long run. Following a prescribed maintenance diet that includes more healthy, high quality lean protein, fresh fruits and vegetables are behaviors that can turn into habits over time. When healthy habits are formed, the risk of regaining weight is reduced.
Implications for Clinical Practice
Although there is evidence demonstrating the efficacy of pharmacological interventions for treating patients with obesity, the side effects of these drugs warrant careful consideration for healthy and successful long-term weight loss and weight management. In a Novo Nordisk-funded study, the authors acknowledge a 45 percent decrease in calories when patients take Semaglutide, as well as changes to their taste preferences.11 In lieu of medications with Semaglutide as the active ingredient, health care professionals should work with patients to develop a healthy and sustainable weight loss plan that meets patients nutritional requirements, fosters behavior change and addresses physical activity needs.
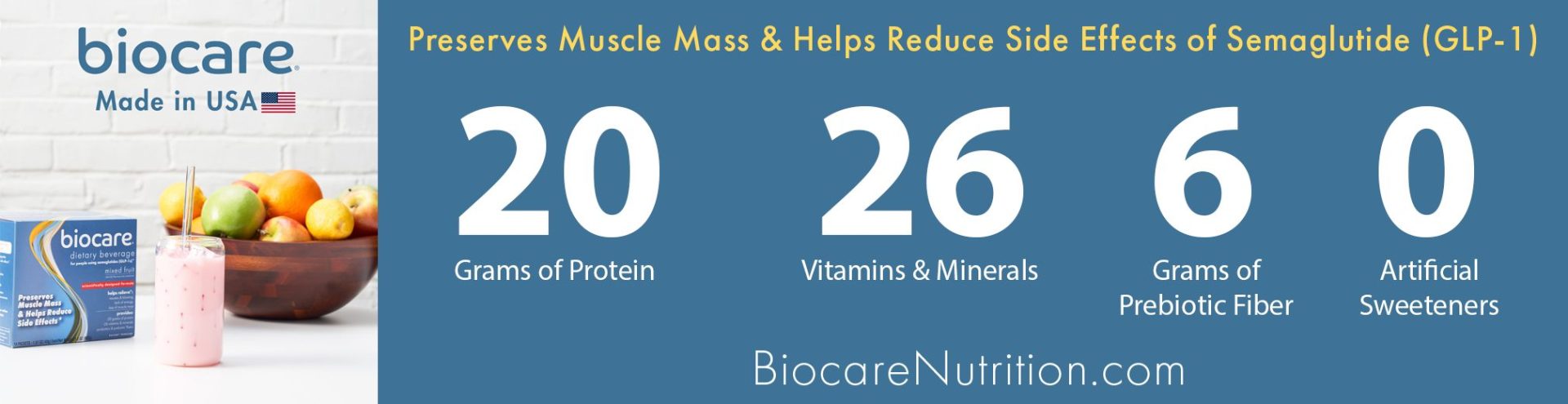
A sustainable healthy plan should include meal replacements as part of a low calorie diet. Meal replacements can provide 15-25 grams of protein, three to six grams of dietary fiber, vitamins and minerals — per serving — to ensure daily nutritional needs are being met and weight loss is happening at a healthy, sustainable pace. A healthy, sustainable weight loss plan should also include a tailored physical activity program that will work hand-in-hand with a low calorie diet. When diet, exercise and behavior education are combined, weight loss and weight management unfold at a healthier and more sustainable pace while avoiding the side effects of anti-obesity drugs.
Sources:
1 Some people taking weight loss drugs say they’re experiencing hair loss
3 How new weight loss drugs are changing the conversation around treating obesity
4 Good luck paying for those $10,000 obesity drugs everyone’s talking about
7 Diet and exercise in management of obesity and overweight
8 State of obesity 2022: Better policies for a healthier America
9 World obesity atlas 2023 press release
10 A systematic review and meta‐analysis of the effectiveness of meal replacements for weight loss
11 Anti-obesity medications and the importance of meeting nutritional requirements
About the Author: Dr. Dawn M. Sweet has over 20 years of experience in the field of communication. Sweet has given several invited talks to and workshops for academic and private sector audiences on the role of nonverbal and verbal communication in achieving positive outcomes and mitigating bias. Her research has been published in several top ranked peer-review journals, and it has been featured on NPR’s River to River / All Things Considered, Buzzfeed, and Science Daily. Her research has also been used to inform expert testimony.




